Worsening Symptoms
Increased Dyspnea (Shortness of Breath): This is often the most prominent symptom, ranging from mild breathlessness to severe air hunger.
Wheezing: A high-pitched whistling sound, particularly on exhalation, due to narrowed airways.
Cough: Can be dry or productive, often worsening at night or with activity.
Chest Tightness: A constrictive feeling across the chest.
Reduced Exercise Tolerance: Inability to perform usual activities without symptoms.
Increased Nocturnal Symptoms: Waking up due to asthma symptoms is a significant red flag for worsening control and potential exacerbation.
and Clinical Manifestations
Objective Measures of Worsening Lung Function
Decreased Peak Expiratory Flow (PEF) or Forced Expiratory Volume in 1 Second (FEV1): These objective measures, particularly a fall from a patient's personal best, confirm airway obstruction and its severity. A drop of 20% or more is often indicative of an exacerbation.
Increased SABA Use: A patient requiring more frequent doses of their short-acting beta-agonist (SABA) reliever (like salbutamol) is a hallmark sign of deteriorating control and an impending or active exacerbation.
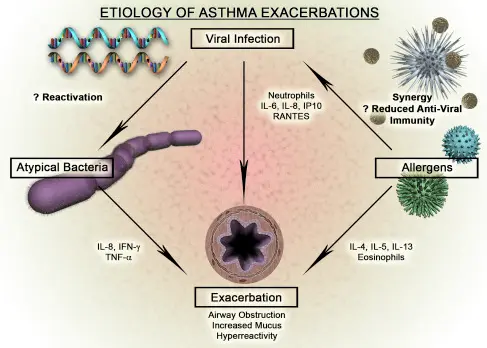
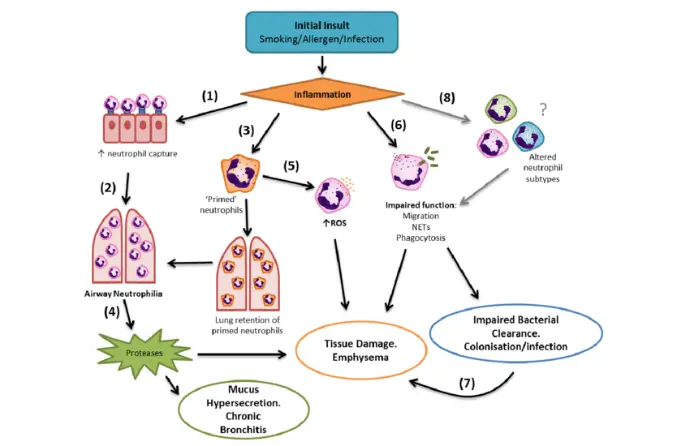
Underlying Pathophysiology: Why Do They Happen?
Asthma exacerbations are primarily driven by an acute increase in airway inflammation and bronchoconstriction.
Airway Inflammation:
Infiltration of inflammatory cells (eosinophils, neutrophils, lymphocytes, mast cells).
Release of inflammatory mediators (cytokines, leukotrienes, histamine).
Leads to mucosal edema (swelling of the airway lining), increased mucus production (often thick and tenacious), and shedding of epithelial cells.
This inflammation narrows the airway lumen and makes it hyperresponsive to stimuli.
Bronchoconstriction:
Acute spasm of the smooth muscle surrounding the airways, triggered by inflammatory mediators and neuronal reflexes.
This rapid narrowing is what salbutamol directly targets.
Airway Remodeling (in chronic severe asthma):
While not the cause of an acute exacerbation, chronic, poorly controlled inflammation can lead to permanent structural changes in the airways (e.g., thickening of the airway wall, increased smooth muscle mass), making them less responsive to treatment over time and potentially more prone to severe exacerbations.

Hook: Start with the significant impact of asthma exacerbations on patient quality of life, healthcare burden, and even mortality.

Briefly Define: What is an asthma exacerbation? (Acute worsening of symptoms, often requiring increased medication or emergency care).

Introduce Salbutamol: Acknowledge its long-standing, critical role as the primary "reliever" medication due to its rapid bronchodilatory effect.

Thesis Statement: While essential, contemporary understanding and guidelines are prompting a critical re-evaluation of salbutamol's place, particularly concerning overuse and the evolving role of anti-inflammatory relief.
- Mechanism of Action (Brief & Clear): Beta-2 adrenergic agonist, leading to smooth muscle relaxation and bronchodilation. Explain why it works fast.
- Clinical Efficacy: Undeniable rapid symptom relief.
- The "Rescue" Paradox: Explain how its effectiveness can inadvertently lead to overuse.
- Problem 1: Masking Worsening Inflammation: Over-reliance on salbutamol can mask the underlying inflammatory process, delaying appropriate escalation of controller therapy.
- Problem 2: Adverse Effects of Overuse:
- Tachycardia, tremors, hypokalemia (briefly mention why these occur).
- Potential for desensitization of beta-2 receptors with chronic high-dose use, potentially reducing effectiveness when truly needed.
- Increased risk of adverse asthma outcomes (hospitalizations, even death) linked to frequent SABA use (cite evidence if possible, e.g., "studies have shown a correlation...").
The Paradigm Shift: GINA and the Emphasis on Anti-Inflammatory Relief
1
Introduce GINA (Global Initiative for Asthma):
Explain its role as the leading international guideline body.
2
The Key Change:
Highlight GINA's recommendations since 2019/2021 to move away from SABA monotherapy for relief in Steps 1-2.
3
Why the Shift?
Recognition that all asthma, even mild, has an inflammatory component.
The understanding that SABA alone does not address inflammation.
The benefits of combining a SABA with an inhaled corticosteroid (ICS) or using an ICS-formoterol combination as a reliever.
4
Introduce ICS-Formoterol (SMART/AIRP):
Explain what it is (Fixed combination of an ICS and a fast-acting LABA).
Mechanism: Provides both bronchodilation (formoterol) and anti-inflammatory action (ICS) at the point of symptom relief.
Benefits: Shown to reduce exacerbation rates, improve symptom control, and lower overall steroid exposure compared to SABA-only relief in milder asthma.
Contemporary Management Strategies: Where Does Salbutamol Fit Now?
Controlled Use: Salbutamol remains crucial for true rescue in moderate-to-severe exacerbations, especially in hospital settings or when immediate, potent bronchodilation is paramount.
As-Needed ICS-Formoterol: For many patients (especially Steps 1-3), ICS-formoterol as a reliever is now preferred.
Regular Controller Therapy is King: Reiterate that optimal daily controller therapy (e.g., daily ICS, LABA/ICS combinations) is the cornerstone of preventing exacerbations. Salbutamol's role is complementary, not primary.
Personalized Approach: Emphasize that management must be tailored to the individual patient's asthma severity, control level, adherence, and preferences.